
Select any field (letters A–J) for details on how to complete each ABN section.
The Advance Beneficiary Notice of Non-coverage (ABN), Form (CMS-R-131) helps Medicare Fee-for-Service (FFS) patients make informed decisions about items and services Medicare usually covers but may not in specific situations. For example, the items or services may not be medically necessary for a patient.
When health care providers and suppliers expect a Medicare coverage denial for a service we generally cover, they must issue an ABN to transfer the financial liability to the patient, including:
This educational tool shows health care providers and suppliers how to correctly complete an ABN form. In this ABN tutorial, you refers to the provider or supplier issuing the form, while on the ABN form, you refers to the patient signing it.

You must issue an ABN:
We may hold you financially liable if you don’t give the patient an ABN in these situations.
Don’t use an ABN for Medicare Advantage (Part C) or Medicare Prescription Drug Benefit (Part D) items and services.
You don’t need to notify the patient before you provide items or services that aren’t a benefit or never covered. Section 20.2 of the Medicare Claims Processing Manual, Chapter 30 has a list of items and services Medicare doesn’t cover.
We recommend issuing a voluntary ABN or a similar notice as a courtesy to alert the patient about their financial liability.
An ABN is valid if you:
If the patient or their representative refuses to choose an option or sign the ABN, note the refusal on the original ABN. You can list refusal witnesses, but it’s not required. If a patient refuses to sign a properly issued ABN, consider not providing the item or service unless the consequences (health and safety of the patient or civil liability in case of harm) prevent it.
In this tutorial, select any field (letters A–J) for details on how to complete each ABN section.
Entities who issue ABNs are collectively known as “notifiers,” which can include physicians, practitioners, providers (including labs) and suppliers, and utilization review committees.
If you reproduce the ABN, remove the letters before issuing it to the patient.
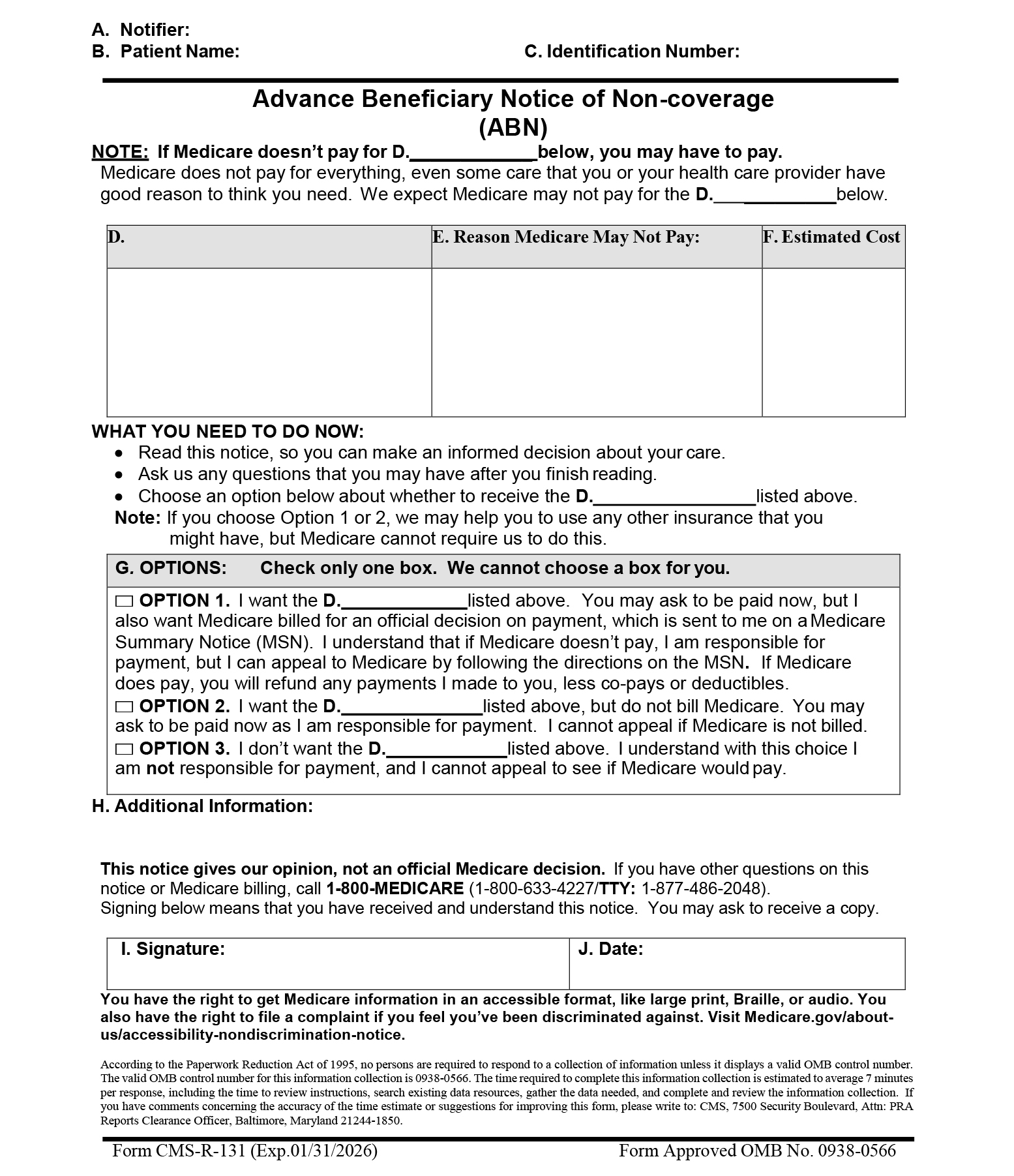
You must enter the patient’s first and last name and include a middle initial if it appears on their Medicare card. We won’t invalidate the ABN because of a misspelling or missing initial if the patient or representative recognizes the name listed on the notice as the patient’s.
This field is optional. Having no identification number doesn’t invalidate the ABN. You may enter a patient identification number that links the notice with a related claim, and you may create an internal filing number, like a medical record number. Don’t list MBIs or SSNs on the notice.
List 1 of these descriptors:
Use the same wording used in the first (D) field.
Use the same wording used in the first (D) field.
In this column, notifiers must explain, in patient-friendly language, why they believe we may not cover the items or services in column (D). We commonly use these non-coverage reasons:
To be a valid ABN, you must list at least 1 reason for each item or service in column (D). You can use the same non-coverage reason for multiple items in column (D) when appropriate.
Complete the 3 (D) fields under the (G) Options section with the same wording used in the first (D) field. The patient, or their representative, must choose 1 of the 3 options listed. We don’t allow you to make this selection.
Special guidance for people who are dually enrolled in both Medicare and Medicaid, also known as dually eligible individuals (has a Qualified Medicare Beneficiary (QMB) Program or Medicaid coverage), ONLY:
Instruct them to check ABN Option Box 1 so the notifier can submit the claim for Medicare adjudication. Strike through Option Box 1 language as shown here:
□ OPTION 1. I want the D._______ listed above. You may ask to be paid now, but I also want Medicare billed for an official decision on payment, which is sent to me on a Medicare Summary Notice (MSN). I understand that if Medicare doesn’t pay, I am responsible for payment, but I can appeal to Medicare by following the directions on the MSN. If Medicare does pay, you will refund any payments I made to you, less co-pays or deductibles.
We require these edits because the notifier can’t bill the dually eligible patient when they offer an ABN. You can’t bill the patient pending Medicare and Medicaid adjudication because federal law affects dually eligible patient coverage and billing.
If we deny a claim when you needed an ABN to transfer financial liability to the patient, cross the claim over to Medicaid or submit it for adjudication based on state Medicaid coverage and payment policy. Medicaid will issue a remittance advice based on this determination. Once Medicare and Medicaid adjudicate the claim, you may only charge the patient in these circumstances:
Note: The patient doesn’t need to check an option box or sign and date the notice when you issue the ABN as a voluntary notice.
The patient wants to get the items or services listed and accepts financial responsibility if we don’t pay. They agree to pay now, if required. Notifiers must submit a claim to Medicare that results in a payment decision the patient can appeal. If they need a Medicare claim denial for secondary insurance to cover the service, advise them to select Option 1.
Special guidance for non-participating suppliers and providers (those who don’t accept Medicare assignment) ONLY:
Strike the last Option Box 1 sentence as shown here:
□ OPTION 1. I want the D. ___________ listed above. You may ask for payment now, but I also want Medicare billed for an official decision on payment, sent to me, on a Medicare Summary Notice (MSN). I understand if Medicare doesn’t pay, I am responsible for payment, but I can appeal to Medicare by following the MSN directions. If Medicare does pay, you will refund any payments I made to you, less co-pays or deductibles.
Notifiers include this single line strike on ABNs printed specifically when you provide unassigned items and services. You can also hand-pen the line on an already-printed ABN. Don’t entirely conceal or delete the sentence. We don’t require you or patients to initial beside the sentence or date the annotations when you make the changes.
When you strike this sentence, include this CMS-approved unassigned claim statement in the (H) Additional Information section:
“This supplier doesn’t accept Medicare payment for the item(s) listed in the table above. If I checked Option 1 above, I am responsible for directly paying the supplier’s charge for the item(s). If Medicare does pay, Medicare will pay me the Medicare-approved amount for the item(s), and this payment may be less than the supplier’s charge.”
You can include this statement on ABNs printed for unassigned items and services or hand-write it in a legible 10 point or larger font.
Use the same wording used in the first (D) field.